 In 1978, the birth of Louise Brown heralded a new era in reproductive medicine. Since then, over eight million babies have been born through this once 'revolutionary procedure. While in vitro fertilization (IVF )was originally designed to bypass blocked or damaged fallopian tubes, its application has been extended to male factor infertility, unexplained infertility, and failure of conventional treatment such as ovulation induction with intrauterine insemination.
In 1978, the birth of Louise Brown heralded a new era in reproductive medicine. Since then, over eight million babies have been born through this once 'revolutionary procedure. While in vitro fertilization (IVF )was originally designed to bypass blocked or damaged fallopian tubes, its application has been extended to male factor infertility, unexplained infertility, and failure of conventional treatment such as ovulation induction with intrauterine insemination.
The IVF process involves stimulation of the ovaries to develop and obtain multiple eggs and removing those eggs by ultrasound-guided needle aspiration. The patient is given anesthesia for the procedure, which takes fifteen to twenty minutes.
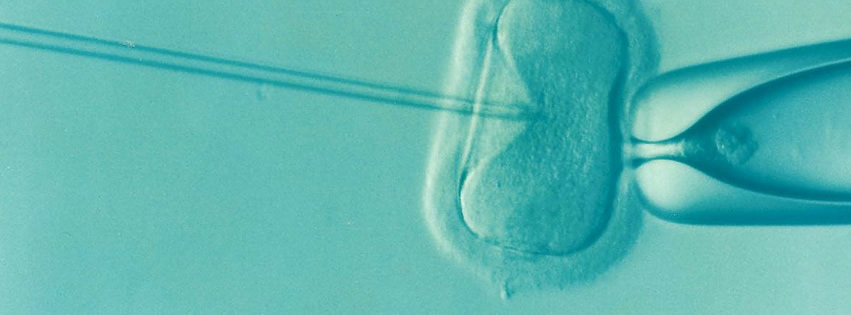
After the eggs are isolated in the laboratory and the partner's sperm is prepared, the eggs are either inseminated or injected with the sperm. The resulting embryos are cultured in the incubator and evaluated daily.
The doctor returns the embryos, via a thin, soft catheter, to the uterus in three to five days. Blastocysts are embryos in a more advanced state of development, commonly developed by the fifth day in culture. Blastocysts are often the hardiest embryos and are more likely to be of good quality.
In 1978, the first baby who was conceived through in vitro fertilization was born in London. Over 40 years later, IVF has become a common and recommended option for some couples struggling with infertility. IVF is when the egg is removed from the intended female parent or the egg donor and combined in a petri dish with the sperm of the intended male parent or a donor. Ideally the sperm and the egg will form an embryo that our laboratory will monitor for a few days for viability. The viable embryo will then be placed in the intended female parent or surrogate. Dr. Blotner discusses when IVF is an appropriate option for patients hoping to build their family.
When is IVF the Best Option?
Impaired Fallopian Tube
Doctors initially designed IVF for tubal obstruction patients diagnosed by HSG or a previous laparoscopy. Damaged tubes, or in some cases, patients who had their tubes removed due to excessive scarring or previous ectopic pregnancy, had little hope of conceiving. The development of IVF allowed the egg to surpass the tube, become fertilized, and be placed safely back into the uterus. We recommend IVF for patients with tubal abnormalities.
Uterine Issues
Some medical issues can make it impossible for a woman to carry a child to term. Diseases such as cancer and adenomyosis can cause a woman to lose her uterus prematurely. There are even cases where women are born without a uterus or have severe uterine defects. For women with healthy egg reserves, IVF allows women who do not have the option of carrying their child to contribute genetically to their offspring. A patient's eggs can be extracted from the intended female parent during an IVF cycle and combined with the intended male parent or sperm donor to form an embryo. We then transfer the embryo to a gestational carrier. For gay male couples, IVF allows the use of an egg donor and a gestational carrier, which lets the intended fathers contribute genetically to their child.
Low Ovarian Reserve
There are a few factors that could diminish a patient's ovarian reserve. A patient's age, a genetic factor contributing to low ovarian reserve, or an autoimmune disorder are reasons why a patient may not have a high ovarian reserve. We usually recommend IVF for these patients for a greater chance of conceiving. For some patients with severely diminished ovarian reserve, using an egg donor would be another option to explore. When using an egg donor, IVF allows the donor's eggs to be extracted and combined with the sperm of the intended male parent or sperm donor. We then transfer the embryos to the intended female parent.
Read more about In Vitro Fertilization on the RESOLVE website.
Male Factor Infertility
ICSI is a technology that was created after IVF was in practice. Instead of merely combing the eggs and sperm in a dish to fertilize, ICSI is when a single sperm is directly injected into a single egg to help promote fertilization. This technology benefits male patients who have a low sperm count, compromised morphology or motility or problems ejaculating sperm or holding an erection to do an injury or disorder. Once the egg is fertilized, the embryo is assessed for viability and then put back in the intended female parent or gestational carrier.
Chromosomal Issues
Patients who undergo IVF have the added benefit of using CGH, a process of testing embryos for any genetic abnormalities. For patients who have a history of life-threatening genetic diseases in their family or for those who have other chromosomal defects, like a translocation, which can cause recurrent pregnancy loss or can have a devastating effect on the fetus, CGH is an excellent option to help decipher which embryos are viable. After the embryos are tested, only the healthy embryos are placed back into the uterus.
Unexplained Infertility
Some couples never get an answer as to why their attempts to conceive are not working out. According to RESOLVE, it is estimated that one in five couples are diagnosed with unexplained infertility. For these couples, IVF can sometimes be a useful tool. The chances of achieving a healthy pregnancy is 3x times higher using IVF than using IUI. When you place the embryo directly into the uterus it eliminates a lot of variables, such as the sperm having issues finding the egg or wondering if the embryo develops. For couples going through unexplained infertility, IVF can give them a greater chance of conceiving.
In the past 40 years, incredible advances have been made in the field of Reproductive Endocrinology. Dr. Blotner is elated to offer these many tools to his patients trying to conceive. He uses all the latest technologies to try to assist patients in their dreams of achieving a healthy pregnancy.

